Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2025, vol. 24(1), pp. 44–51 DOI: https://doi.org/10.15388/LietChirur.2025.24(1).4
Aesthetic Correction of Gynecomastia with Liposuction and Limited Access Breast Excision – an Experience
Saleh Alhotan
Department of Surgery, College of Medicine, Qassim University, Saudi Arabia
E-mail: saleh.alhotan@gmail.com
ORCID: https://orcid.org/0009-0001-6425-3459
https://ror.org/01wsfe280
Sajad Ahmad Salati
Department of Surgery, College of Medicine, Qassim University, Saudi Arabia
E-mail: docsajad@gmail.com
ORCID: https://orcid.org/0000-0003-2998-7542
https://ror.org/01wsfe280
Abstract. Background. Gynecomastia is the most common breast disorder in males and is characterized by benign enlargement of glandular tissue. Surgical management options are adopted if it fails to resolve spontaneously or if conservative measures are ineffective in alleviating symptoms. Liposuction with limited access mammary gland excision is one such option. Aim of the study. This study was undertaken to study the outcomes of gynecomastia treated with liposuction and limited access mammary gland excision. Methods. The data related to the patients was analysed retrospectively and multiple variables were studied which included the demographics, grading, complications, and patient satisfaction. Results. 85.4% of patients were highly satisfied or satisfied with the outcomes, and 78.9% witnessed significant improvement in psychosocial distress. Minor complications were recorded in 35.4% of cases, and histopathological analysis of retrieved breast tissue specimens revealed benign features in all the patients. Conclusions. There are several surgical treatments for managing gynecomastia that either fails to resolve spontaneously or causes distressing symptoms. Liposuction with limited access mammary gland excision is one such option and is highly successful.
Keywords: gynecomastia, reduction mastectomy, liposuction, hematoma, seroma, Simon’s classification.
Received: 2024-12-29. Accepted: 2025-02-02.
Copyright © 2024 Saleh Alhotan, Sajad Ahmad Salati. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Gynecomastia is defined as a benign proliferation of the glandular tissue of the male breast [1]. The term “gynecomastia” originates from the Greek terms “Gyne”, meaning female, and “mastos”, meaning breast, inferring thereby that, in this condition, a male breast tends to acquire feminine form. It usually affects both the breasts, though it can occur unilaterally [2]. It is a common aesthetic issue and the most common benign breast disorder in males, with a high prevalence rate [3]. A study by Narula and Carlson [4] revealed that some degree of gynecomastia affects 36% of adult young men and 57% of older men, indicating thereby that it affects one in three adult males and one in two elderly men.
Estrogens are known to act as a growth hormone (GH) and stimulate the growth of breast tissue cellular components, whereas androgens inhibit it [5]. Gynecomastia results from an imbalance between androgen and estrogen concentrations that may arise physiologically during growth and development or may be pathologically induced by disease or drugs [6]. Physiologic gynecomastia displays three peak phases [5], correlating to times of higher levels of estrogen, as follows:
1. Neonatal. This occurs during the neonatal period and regresses spontaneously.
2. Adolescent. This occurs during puberty and regresses spontaneously.
3. Elderly. This occurs in older men and is linked to decrease in testosterone production due to testicular aging.
Gynecomastia may manifest unilaterally or bilaterally in each of these populations, and several classification systems have been proposed in the literature for its grading [7–9]. Simon classification [9] is the most accepted system (Figure 1) and hence was adopted for this study.
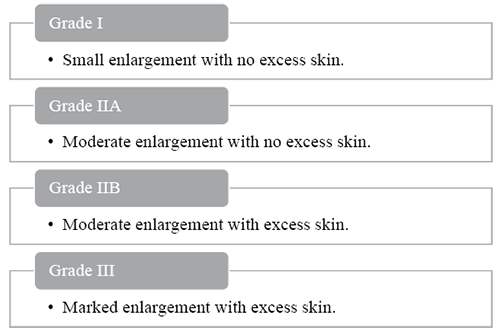
Figure 1. Simon classification of gynecomastia
The excess breast tissue tends to disappear with time; therefore, newborns and adolescent patients often need reassurance and “benign neglect” for at least a year. Adult gynecomastia and unilateral gynecomastia in all age populations usually require further investigational work-up for an underlying secondary cause. When gynecomastia fails to resolve or else causes bothersome symptoms, surgical options are adopted. The objective of this study was to assess the demographic data, grading, surgical technique, complications, and patient satisfaction after surgical management of gynecomastia over a period of five years, using liposuction and limited access mammary gland excision.
Methods
The retrospective study analyzed the cases of gynecomastia managed surgically in the period from January 2019 to January 2024 and followed up for a period of at least one year. The study protocol was approved by the departmental research committee. The data were derived from the verified logbooks of the operating surgeon (SAH). The information recorded included age, symptoms, comorbidities, grade of gynecomastia, location (unilateral or bilateral), management, and the level of satisfaction expressed by the patients. The satisfaction level was assessed at a one-year follow-up with a 5-point Likert scale and recorded as: (1) highly satisfied, (2) satisfied, (3) neither satisfied nor dissatisfied, (4) dissatisfied, (5) highly dissatisfied.
The study followed the ethical principles for medical research involving the human subjects according to the Declaration of Helsinki, and proper informed consent was sought from the patients to use their data for research and publication.
Microsoft Office (MS) Excel 2022 was used for data entry and coding while SPSS (IBM) version 26 was used for data analysis. Frequency and percent were used for describing of categorical variables while mean was used for description of numeric variables.
Surgical technique
The boundaries of the mammary gland and the areas that required liposuction were marked while the patients stood with their feet shoulder-width apart, their eyes fixed straight ahead, their chin up and chest out, and both hands on the respective iliac crests.
Surgical operations were performed under general anesthesia while the patients were in a supine position with their arms in adduction. Prophylactic antibiotics were administered, and total asepsis was achieved. Then, tumescence was achieved by infiltration of 500 ml of saline-adrenaline-xylocaine-tranexamic acid fluid in each breast. Liposuction was conducted using a number 4 rounded-tip liposuction cannula (MicroAire Power Assisted Liposuction System) in the deep fatty tissue in the mammary and perimammary area. A semicircular periareolar incision was made from 3 o’clock to 9 o’clock, and the remnants of the mammary gland were removed via this incision, leaving a small pad of fat under the areola-nipple complex (NAC) measuring about 7 mm to prevent postoperative depression and necrosis of the areola. Touch-up liposuction was then undertaken to remove fat remnants and to even out the inframammary surface to allow better skin redraping and achieve a sculpted chest. No skin excision was undertaken, and pectoral fascia was left intact.
The closure of the periareolar incision was achieved with subcutaneous, interrupted, inverted sutures with undyed Monocryl (Ethicon) 4–0, followed by the application of adhesive surgical tape strips (omni-strips) made of porous non-woven fabric. A pressure dressing was placed after placement of a 16-Fr suction drain. The retrieved specimen of mammary gland was sent for histopathological analysis to obtain a definitive tissue diagnosis. After two to three days, the drain was taken out. Patients were instructed to avoid physical exertion, not to raise their arms above the shoulder, and to wear a custom-made compression garment for 4–6 weeks.
Results
There were 48 patients, ranging in age from 19 years to 68 years (mean 29.7 years), as shown in Table 1.
Table 1. Age distribution of patients
|
Age group (years) |
Number of patients |
Percentage |
|
10–20 |
2 |
4.2% |
|
21–30 |
31 |
64.6% |
|
31–40 |
8 |
16.7% |
|
41–50 |
2 |
4.2% |
|
51–60 |
3 |
6.2% |
|
61–70 |
2 |
4.2% |
|
Total |
48 |
100% |
There were 42 (87.5%) cases of bilateral gynecomastia, and in 6 (12.5%) cases, the disease was unilateral, making a total of 90 breasts. Most cases were asymptomatic (n = 41, 85.4%), and only 7 cases (14.6%) had associated pain/tenderness. Psychological impact manifested as anxiety, depression, and/or low self-esteem was reported in 19 (39.6%) cases. One patient (2.1%) had unilateral testicular agenesis, and one more patient (2.1%) had undergone prostatectomy for carcinoma of the prostate. None of the patients belonged to Grade I; 19 (39.6%), 27 (56.2%), and 2 (4.2%) had Grade IIA, Grade IIB, and Grade III gynecomastia, respectively, as depicted in Figure 2.

Figure 2. Grading of gynecomastia (Simon’s classification)
Preoperatively, all patients were subjected to thorough physical examination, laboratory assessment, bilateral mammary ultrasound, and evaluation at the hands of board-certified urologists and endocrinologists.
There was an uneventful postoperative course in 31 (64.6%) cases (Figure 3). Histopathological analysis of the retrieved specimens of breast revealed benign nature with varying degrees of fibrous, ductal, and fatty tissue. No malignant features were found in any specimen; however, pseudoangiomatous stromal hyperplasia (PASH) and squamous metaplasia were reported in one specimen each. Complications were encountered in 17 (35.4%) but were of minor nature that either resolved spontaneously or else were managed by bedside manoeuvres. These include hematoma (n = 4; 8.3%), cosmetically unpleasant asymmetry (n = 6; 12.5%), paresthesias/numbness in the nipple areola complex or chest wall (n = 3; 6.2%), seroma (n = 3; 6.2%), and skin redundancy (n = 2; 4.2%). Hematomas were managed by evacuation after the release of one or two areolar sutures, whereas seromas were managed by ultrasound-guided aspiration. Skin redundancy and asymmetry were successfully managed with radiofrequency-assisted lipolysis (Inmode BodyTite). 41 (85.4%) patients were either highly satisfied or satisfied with the outcome (Table 2).
Table 2. Level of satisfaction at one year after operation
|
Level of satisfaction |
Number of patients |
Percentage |
|
Highly satisfied |
24 |
50% |
|
Satisfied |
17 |
35.4% |
|
Neither satisfied nor dissatisfied |
5 |
10.4% |
|
Dissatisfied |
2 |
4.2% |
|
Highly dissatisfied |
0 |
0% |
|
Total |
48 |
100% |

Figure 3. A 26-year-old patient with Grade IIB gynecomastia (A to D – preoperative images, E to H – postoperative images at 2 weeks)
Till one-year post-surgery, no patient was advised, nor did any patient (including the dissatisfied ones) request revision surgery. Of the 19 cases with psychological distress, significant improvement was documented in 15 out of 19 (78.9%) cases.
Discussion
Gynecomastia is the most prevalent breast condition in men [3]. Most of the patients are managed conservatively, but due to its very high prevalence, the magnitude of patients seeking surgical management options due to failure of conservative management ends up being quite high. The surgical management options have evolved over the years with the availability of technology and tools, and the focus has gradually shifted from surgical excision to a combination of liposuction and gland excision [10]. This study reports a smaller sample size for gynecomastia management with a combined technique and no skin excision over a period of 5 years; nonetheless, the results are consistent with other studies in the literature.
In this series, 85.4% of cases were asymptomatic, and 14.6% reported pain/tenderness. Psychological distress was manifested in 39.6% of cases, and 78.9% of these cases recorded improvement. These patients had remained under the care of board-certified psychologists after surgery, in addition to our services. In a study conducted by Li et al. [11], 94.8% of patients indicated that having gynecomastia caused them psychological stress. Schonfeld [12] maintained as early as 1961 that both surgery and psychotherapy were required for proper care of gynecomastia due to the way it affected a man’s life. Recent research on adults and teenagers with gynecomastia has proven that it significantly impairs psychosocial factors like self-esteem, mental health, social functioning, and general well-being [13–14]. The primary explanation for this association is that children establish their sexual identity, body image, and self-esteem during adolescence, and that abnormal breast tissue development may have an adverse impact on these domains and act as an anatomic stressor at that phase of life [15].
Complications of minor nature, not requiring any intervention under general anesthesia, were reported in 35.4% of cases, which included hematoma (8.3%), cosmetically unpleasant asymmetry (12.5%), paresthesias/numbness in the nipple areola complex or chest wall (6.2%), seroma (6.2%), and skin redundancy (4.2%). These figures are comparable to other studies in the literature. The overall complication rate was 20.8% and 25.9% in series by Varlet et al. [16] and Ramasamy et al. [17], respectively. Holzmer et al. [10] systematically reviewed 17 studies and reported an overall complication rate of 13.1%, with hematoma (5.8%) being the most common complication, followed by seroma (2.4%). In our series, 85.4% of cases were highly satisfied or satisfied at one year after surgery. In the series by Ramasamy et al. [17] and Brown et al. [1], the satisfaction levels were 93% and 86%, respectively.
All the specimens were reported as benign on histopathological analysis in this series. Histopathological analysis of gynecomastia specimens is mandated by tradition almost universally due to its perceived relationship with malignancy [18–21]. Senger et al. [22] in 2014 questioned the necessity of this routine histopathological analysis of gynecomastia specimens by reviewing the data from the Saskatoon Health Region (Saskatchewan) over a 15-year period and reviewing the literature for evidence-based guidelines. The study did not detect any significant histopathological concerns in 452 gynecomastia cases, and in the context of evidence-based literature, the authors proposed the re-evaluation of the practice of routine histopathological examination of tissue from every gynecomastia.
In our series, no patient required revision surgery, and the adverse effects were minor, requiring office-based intervention. The rate of revision operations varies among published articles in peer-reviewed literature. Sim et al. [23] reported a revision rate of 14%, whereas 7.1% of patients in a series by Ramasamy et al. [17] reported a desire to seek revision operation in the future. Breast asymmetry, insufficient gland removal, nipple migration, and unsightly scars are the common reported indications of revisions. In this series, after liposuction, a semi-circular periareolar incision was made; hence, sufficient access was attained to ensure the retrieval of the gland completely. Furthermore, touch-up liposuction post-gland excision further evacuated gland remnants. Postoperatively, skin redundancy and asymmetry were successfully handled with radiofrequency-assisted lipolysis (Inmode BodyTite). All these measures explain the absence of the need for revision surgery in our series.
The surgical art related to the management of gynecomastia is continuously evolving, and a wide range of procedures have been added to the cosmetic surgical armamentarium in recent years. These management options include transareolar excision of the mammary gland, ultrasonic-assisted lipoplasty with muscular definition, disruption of the inframammary fold, bipolar radiofrequency tightening, Vaser liposuction, pedicled nipple areola complex (NAC) mastopexy with boomerang pattern excision and J torsoplasty, NAC grafts with hockey stick excision pattern, and pectoralis muscle lipoaugmentation [24]. All the available options, including the technique adopted by us, aim at achieving the aesthetic goal of total glandular reduction, proper positioning and shape of the NAC, and masculine chest wall contour.
Limitations
The limitations of this study include relatively smaller sample size and non-availability of consent for recording and publications of images during surgical procedure, while the patient was under anesthesia.
Conclusion
Gynecomastia is the most common benign breast disorder in males and poses a significant challenge to the plastic surgeon. There is a wide range of surgical options available for patients who fail to resolve spontaneously. The combined technique of liposuction followed by mammary gland excision is a viable option with a high success rate with acceptable adverse effects. With thorough preparation and astute patient selection, this technique is expected to result in high levels of satisfaction for both the patient and the treating doctor.
Acknowledgments / Patient consent. The authors thank the patients for allowing the usage of data and images (before and after operation) for research and publication purposes. Patients have consented, with the condition that anonymity would be maintained, and the names and initials would not be published. Furthermore, the patients have not allowed usage of any images taken while they were under anesthesia.
Contribution of authors. SAH is the operating surgeon; he has contributed the data, photos and drafted the methods & surgical technique sections. The other sections of the manuscript have been drafted by SAS. Both the authors have approved the final manuscript.
Financial support and sponsorship. There is no financial support or sponsorship for this project, and it has been undertaken purely for academic, non-commercial purposes.
Conflicts of interest. There are no conflicts of interest.
Data availability. Data can be made available on request, by the corresponding author.
References
1. Brown RH, Chang DK, Siy R, Friedman J. Trends in the surgical correction of gynecomastia. Semin Plast Surg 2015; 29(2): 122–130. DOI: 10.1055/s-0035-1549053.
2. Devalia HL, Layer GT. Current concepts in gynaecomastia. Surgeon 2009; 7(2): 114–119. DOI: 10.1016/s1479-666x(09)80026-7.
3. Fagerlund A, Lewin R, Rufolo G, Elander A, Santanelli di Pompeo F, Selvaggi G. Gynecomastia: a systematic review. J Plast Surg Hand Surg 2015; 49(6): 311–318. DOI: 10.3109/2000656X.2015.1053398.
4. Narula HS, Carlson HE. Gynaecomastia: pathophysiology, diagnosis and treatment. Nat Rev Endocrinol 2014; 10(11): 684–698. DOI: 10.1038/nrendo.2014.139.
5. De Medeiros MMM. Surgical approach to the treatment of gynecomastia according to its classification. Rev Bras Cir Plást 2012; 27(2): 277–282.
6. Deepinder F, Braunstein GD. Drug-induced gynecomastia: an evidence-based review. Expert Opin Drug Saf 2012; 11(5): 779–795.
7. Monarca C, Rizzo MI. Gynecomastia: tips and tricks-classification and surgical approach. Plast Reconstr Surg 2013; 131(5): 863e–865e. DOI: 10.1097/PRS.0b013e318287a18f.
8. Waltho D, Hatchell A, Thoma A. Gynecomastia classification for surgical management: a systematic review and novel classification system. Plast Reconstr Surg 2017; 139(3): 638e–648e. DOI: 10.1097/PRS.0000000000003059.
9. Simon BE, Hoffman S, Kahn S. Classification and surgical correction of gynecomastia. Plast Reconstr Surg 1973; 51(1): 48–52. DOI: 10.1097/00006534-197301000-00009.
10. Holzmer SW, Lewis PG, Landau MJ, Hill ME. Surgical management of gynecomastia: a comprehensive review of the literature. Plast Reconstr Surg Glob Open 2020; 8(10): e3161. DOI: 10.1097/GOX.0000000000003161.
11. Li CC, Fu JP, Chang SC, Chen TM, Chen SG. Surgical treatment of gynecomastia: complications and outcomes. Ann Plast Surg 2012; 69(5): 510–515. DOI: 10.1097/SAP.0b013e318222834d.
12. Schonfeld WA. Gynecomastia in adolescence. Personality effects. Arch Gen Psychiatry 1961; 5: 46–54. DOI: 10.1001/archpsyc.1961.01710130048006.
13. Nuzzi LC, Cerrato FE, Erikson CR, Webb ML, Rosen H, Walsh EM, DiVasta AD, Greene AK, Labow BI. Psychosocial impact of adolescent gynecomastia: a prospective case-control study. Plast Reconstr Surg 2013; 131(4): 890–896. DOI: 10.1097/PRS.0b013e3182818ea8.
14. Nuzzi LC, Cerrato FE, Webb ML, Faulkner HR, Walsh EM, DiVasta AD, Greene AK, Labow BI. Psychological impact of breast asymmetry on adolescents: a prospective cohort study. Plast Reconstr Surg 2014; 134(6): 1116–1123. DOI: 10.1097/PRS.0000000000000736.
15. Kinsella C Jr, Landfair A, Rottgers SA, Cray JJ, Weidman C, Deleyiannis FW, Grunwaldt L, Losee JE. The psychological burden of idiopathic adolescent gynecomastia. Plast Reconstr Surg 2012; 129(1): 1–7. DOI: 10.1097/PRS.0b013e3182361efd.
16. Varlet F, Esposito C, Scalabre A, Lepore B, Vermersch S, Escolino M. Pediatric endoscopic subcutaneous mastectomy [pesma] with liposuction in adolescents with gynecomastia. Surg Endosc 2023; 37[1]: 766–773. DOI: 10.1007/s00464-022-09550-x.
17. Ramasamy K, Tripathee S, Murugesh A, Jesudass J, Sinha R, Alagarasan AR. A single-center experience with gynecomastia treatment using liposuction, complete gland removal, and nipple areola complex lifting plaster technique: a review of 448 patients. Aesthet Surg J Open Forum 2023; 5: ojac095. DOI: 10.1093/asjof/ojac095.
18. Ucak R, Tank C, Kabukcuoglu F. Incidence of atypical change and risk of breast cancer in patients with gynecomastia. Iranian Red Crescent Medical Journal (IRCMJ) 2022; 24(7). DOI: 10.32592/ircmj.2022.24.7.1443.
19. Liao EC, Kish JB, Hertl MC. Incidental discovery of bilateral breast cancer in a 24-year-old man presenting with gynecomastia. Ann Plast Surg 2007; 58(6): 673–676. DOI: 10.1097/01.sap.0000245118.98550.cf.
20. Wadie GM, Banever GT, Moriarty KP, Courtney RA, Boyd T. Ductal carcinoma in situ in a 16-year-old adolescent boy with gynecomastia: a case report. J Pediatr Surg 2005; 40(8): 1349–1353. DOI: 10.1016/j.jpedsurg.2005.05.026.
21. Lemoine C, Mayer SK, Beaunoyer M, Mongeau C, Ouimet A. Incidental finding of synchronous bilateral ductal carcinoma in situ associated with gynecomastia in a 15-year-old obese boy: case report and review of the literature. J Pediatr Surg 2011; 46(9): e17–20. DOI: 10.1016/j.jpedsurg.2011.06.010.
22. Senger JL, Chandran G, Kanthan R. Is routine pathological evaluation of tissue from gynecomastia necessary? A 15-year retrospective pathological and literature review. Plast Surg (Oakv) 2014; 22(2): 112–116.
23. Sim N, Tan G, Tan BK, Goh T. Review of the microdebrider excision and liposuction technique (MELT) for the treatment of gynecomastia. J Plast Reconstr Aesthet Surg 2020; 73(2): 303–312. DOI: 10.1016/j.bjps.2019.09.003.
24. Hurwitz DJ, Davila AA. Contemporary management of gynecomastia. Clin Plast Surg 2022; 49(2): 293–305. DOI: 10.1016/j.cps.2021.12.003.